What the U.S. Must Do Now To Avoid the Next Pandemic
Lifecycle Management & Modernization, Health, Pandemic Response Support, Risk Management, Agile Project Management, Artificial Intelligence, Health SecurityCOVID-19 is not the first pandemic the United States has faced, but it may be the one that teaches us some very modern lessons about public trust, our surveillance networks, and effective response management. Here’s what the U.S. can learn from past pandemics and COVID-19 to ensure an effective response to the next pandemic.
Comprehensive Pandemic Threat Assessment as an Ongoing Effort
During and immediately after a pandemic or biological threat, there is often support among a variety of stakeholders to fund surveillance efforts. But, much like you can’t win the next war by fighting the last one, creating an overly optimized response to the most recent threat produces the risk of creating an ultimately ineffective plan. Ebola, for example, is not transmitted the same way as COVID-19. Comprehensive response requires a deep understanding of all threats. In this way, preventing the next pandemic should be viewed as an ongoing research-and-resiliency effort within federal agencies.
Successful research-and-resiliency work includes assessing the efficacy of plans as well as creating consistent funding for biological surveillance, drug testing, and development. One of the COVID-19 response successes has been identifying therapeutics that limit the runaway immune response that causes severe COVID-19. Through Operation Warp Speed and other efforts, researchers were empowered to rapidly test therapeutics and use novel approaches, such as mRNA technology, to create vaccines.
But, consider the time and lives that could’ve been saved if virus detection and prevention was consistently funded and prioritized.
“In the U.S. right now, we have a strong network in place for surveillance of influenza and building vaccines each year in response,” explained Dr. Catherine Bigger, an LMI principal technical advisor in biology. “The fact that coronaviruses exhibit the same evolution potential as influenza suggests the need for an ongoing surveillance like what we have in place for the flu. There is an opportunity to build on this work and expand the capability of the network.”
“The fact that coronaviruses exhibit the same evolution potential as influenza suggests the need for an ongoing surveillance like what we have in place for the flu. There is an opportunity to build on this work and expand the capability of the network.”
For that network to succeed, additional sequencing and testing is critical. The U.S. has fallen significantly behind other countries in its sequencing of coronavirus variants. According to the GISAID global database, the U.S. is only sequencing the genome in as little as 0.3% of positive cases compared to over 10% in other countries. Sequencing in other countries has helped to identify new strains that allow countries to get ahead of the outbreak, but this is work that should be done domestically as well—and not just with coronaviruses.
Dr. Shanmuga Sozhamannan, a fellow in science and technology at LMI, has direct experience in sequencing and notes that the U.S. has much of the infrastructure in place to rapidly expand surveillance. “What is lacking is a coordinated effort at the federal level to use what we have,” he said. “That’s where policymakers can step in and work with researchers, the Centers for Disease Control and Prevention, and private-sector consultants to develop guidelines and support information sharing. Recent trends in ramped up sequencing of COVID samples in the U.S. are encouraging, and the key is to maintain this infrastructure post-COVID for the next pandemic.”
Leveraging Artificial Intelligence and Other Technologies as Force Multipliers
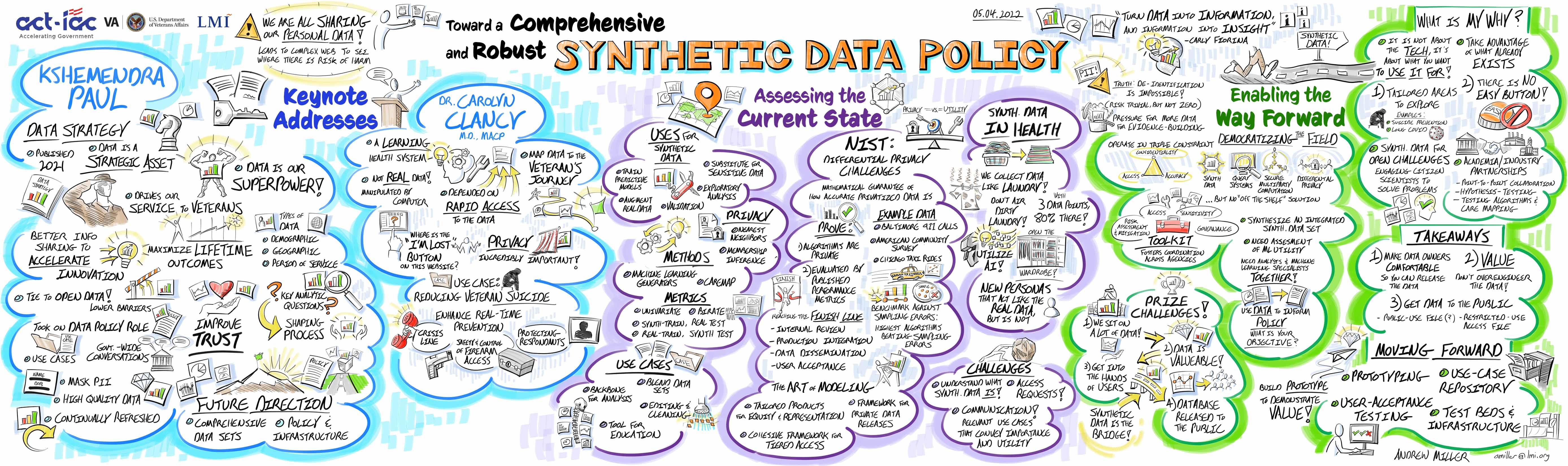
Effective pandemic planning requires significant biological and logistical data management. Artificial intelligence, data analytics, and other technologies can be force multipliers during the modeling and planning phases. In this way, stakeholders gain visibility into hospital capacity, vulnerable populations, and emergent biological threats before diseases become difficult to contain. The efforts to combine and synthesize these data that occurred during COVID-19 must be continued to better provide a holistic view to a multitude of stakeholders.
This information can also help to bolster national stockpiles of personal protective equipment, therapeutics, and other necessary medical apparatus. Data analytics are widely deployed throughout the private sector to monitor inventory stock and replenishment needs. Organizations such as the Strategic National Stockpile are now looking to increase awareness of available resources and enable the understanding of the gaps that exist, both within government and private industry.
Dr. John Bigger, a principal technical advisor and biologist at LMI, noted the importance of the federal government’s role as a resource hub. “There is always going to be a lag while the medical and scientific communities understand the threat and identify appropriate treatments,” he said. That lag becomes exacerbated when the supply chain from both private- and public-sector sources can’t meet the demands in a timely manner. To combat this, public and private sectors must work together to build a resilient supply chain capable of meeting a wide variety of scenarios in an uncertain environment and reduce the time to impact and time to recovery.
Supporting a Collective Response to Public Health Threats
A network of scientific researchers, public health experts, and private-sector partners is available to respond to emerging viral threats. Without a coordinated response, however, no network can be effective. Using the framework of the influenza surveillance network is an option, but it is also important to build permanency into the network. In practical terms, this means supporting targeted and permanent federal funding as part of national resiliency efforts. It also means rebuilding public trust in institutions and science in general.
The CDC and other federal agencies have mounted successful public information campaigns for additional health issues. It’s worth exploring an ongoing public education effort to combat misinformation and improve understanding around vaccines and therapeutics for COVID-19 and other emergent viruses. Agencies can work with private-sector partners to create targeted education and outreach campaigns.
A Multifaceted, Ongoing Response for Successful Pandemic Preparedness
When threats to public health are largely under control, it can be hard to maintain momentum for testing, tracing, and surveillance. Thinking about pandemic response as a set of permanent, continuous research and development efforts can ensure that the U.S. is always prepared for a multitude of threats. Building on networks can make these efforts more efficient, as can using new technologies. Finally, supporting a collective public-private response to public health through effective education and outreach will instill public trust in the treatments and preventative measures we must take to remain healthy.